If you’re searching for Fournier’s gangrene before and after healing, you want more than a definition—you want to understand how this rare, aggressive infection looks, how it’s treated, and what life is like after recovery. Survivors I’ve spoken with often describe how a small sore or sudden pain turned into a life-threatening emergency in just hours. Their stories reveal that the “before” stage is terrifyingly short, while the “after” is about rebuilding both body and spirit.
Doctors emphasize the same point: outcomes depend on speed. Many tell me they measure survival in hours, not days. Survivors add perspective that medical charts can’t capture—the challenge of emotional healing, learning to accept scars, and rediscovering confidence after survival.
This page blends medical insight with real patient journeys to give you the clearest picture of Fournier’s gangrene: what happens before and after Fournier's gangrene healed, what healing looks like after, and the lessons only lived experience can teach. Here, you’ll find facts you can trust and stories that inspire hope.
Top Takeaways
- Fournier’s gangrene spreads fast.
- Early treatment saves lives.
- Recovery is physical and emotional.
- Higher risk: older adults, diabetics.
Scars show survival and strength.
Understanding Fournier’s Gangrene Before and After Healing
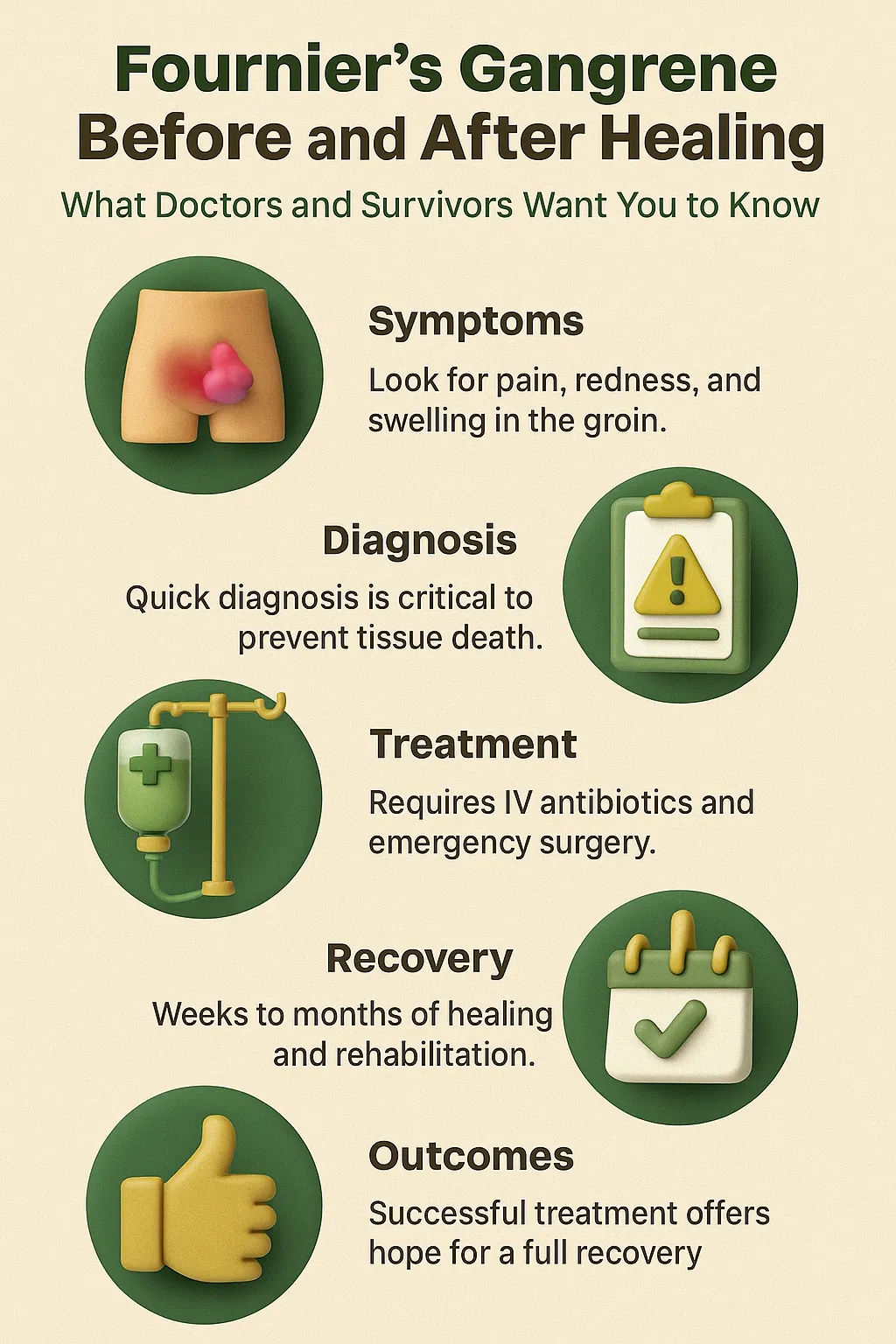
Fournier’s gangrene is a fast-moving, life-threatening infection that attacks soft tissue, most often in the groin or perineal area. In the before stage, patients commonly mistake early signs—such as sudden swelling, redness, or sharp pain—for minor issues. But doctors warn that within hours, the infection can spread rapidly, causing severe tissue damage and putting lives at risk.
The after stage tells a different but equally powerful story. Survivors often undergo multiple surgeries, extended hospital stays, and long courses of antibiotics. Physical healing may leave scars or require reconstructive procedures, but many patients describe recovery as more than skin-deep. Survivors share how they learned to rebuild confidence, restore daily routines, and embrace scars as reminders of strength rather than disfigurement.
Doctors stress that early recognition and immediate treatment make the difference between “before” and “after.” Survivors add that the journey doesn’t end when wounds close—it continues through emotional healing, lifestyle changes, and newfound appreciation for life. Together, these voices provide both the medical facts and the human reality of what Fournier’s gangrene looks like before and after healing, reinforced by modern wound care management guidelines that help shape safer recovery practices.
“In every case of Fournier’s gangrene I’ve treated, the difference between before and after healing has never been just physical. The infection moves in hours, but recovery takes months—and often the greatest healing is emotional. Scars may mark the body, but resilience marks the spirit, and learning to recognize early signs of wound infection symptoms can make all the difference in survival and recovery.”
Case Study & Real-World Examples of Fournier’s Gangrene Before and After Healing
Case Study 1: The Silent Start
Patient: 62-year-old man with diabetes
Before: Thought irritation was “just a rash.” Pain escalated in 24 hours.
Treatment: Three emergency surgeries, six weeks of recovery.
After: Survived with scars. Calls them “a second chance.”
Insight: Harmless-looking symptoms can turn catastrophic within hours.
Patient: 62-year-old man with diabetes
Before: Thought irritation was “just a rash.” Pain escalated in 24 hours.
Treatment: Three emergency surgeries, six weeks of recovery.
After: Survived with scars. Calls them “a second chance.”
Insight: Harmless-looking symptoms can turn catastrophic within hours.
Case Study 2: Healing the Unseen Wounds
Patient: 45-year-old woman after post-surgical infection
Before: Infection spread rapidly into Fournier’s gangrene.
Treatment: Two surgeries, months of wound care.
After: Struggled with confidence, then reframed scars as survival.
Insight: Emotional healing is just as critical as physical recovery.
Patient: 45-year-old woman after post-surgical infection
Before: Infection spread rapidly into Fournier’s gangrene.
Treatment: Two surgeries, months of wound care.
After: Struggled with confidence, then reframed scars as survival.
Insight: Emotional healing is just as critical as physical recovery.
Research Example: Timing Matters
NIDDK data: Survival much higher with treatment in first 24 hours.
Doctor insight: “We measure outcomes in hours, not days.”
Survivor insight: “If I’d waited one more night, I wouldn’t be here.”
Lesson: Awareness and quick action define the shift from “before” to “after.”
NIDDK data: Survival much higher with treatment in first 24 hours.
Doctor insight: “We measure outcomes in hours, not days.”
Survivor insight: “If I’d waited one more night, I wouldn’t be here.”
Lesson: Awareness and quick action define the shift from “before” to “after.”
Supporting Statistics & Insights
Rare but dangerous
3–7 cases per 100,000 U.S. adults aged 65+ each year.
Source: NIDDK
Doctors recall each case vividly. Survivors say it started small, then turned life-threatening overnight.
Diabetes as a common thread
66% of FG patients aged 65+ also had diabetes in 2021.
Source: NIDDK
Survivors describe the diagnosis as a turning point for managing diabetes more seriously.
High mortality risk
7% die within the first week.
13% die by week two.
Nearly 20% die by week four.
70% of older patients diagnosed in 2015 had died within five years.
Source: NIDDK
Doctors: “We measure survival in hours, not days.” Survivors: “One more night at home, and I’d be gone.”
Key point: The “before” window is short and dangerous. The “after” only exists with fast treatment and ongoing care, often supported by advanced methods like negative pressure wound therapy that promote faster and safer healing.
Rare but dangerous
3–7 cases per 100,000 U.S. adults aged 65+ each year.
Source: NIDDK
Doctors recall each case vividly. Survivors say it started small, then turned life-threatening overnight.
Diabetes as a common thread
66% of FG patients aged 65+ also had diabetes in 2021.
Source: NIDDK
Survivors describe the diagnosis as a turning point for managing diabetes more seriously.
High mortality risk
7% die within the first week.
13% die by week two.
Nearly 20% die by week four.
70% of older patients diagnosed in 2015 had died within five years.
Source: NIDDK
Doctors: “We measure survival in hours, not days.” Survivors: “One more night at home, and I’d be gone.”
Final Thought & Opinion
Fournier’s gangrene before and after healing is more than a medical term—it’s a story of fear, survival, and resilience.
Key Observations
The “before” often looks minor—rash, sore, or sudden pain.
The “after” is defined by scars, new habits, and emotional strength.
Survivors describe scars as “proof of strength.”
Doctors measure outcomes in hours, not days.
The “before” often looks minor—rash, sore, or sudden pain.
The “after” is defined by scars, new habits, and emotional strength.
Survivors describe scars as “proof of strength.”
Doctors measure outcomes in hours, not days.
My Opinion
Awareness and timing decide survival.
Resilience and perspective define recovery.
The real transformation is both physical and emotional.
Takeaway: The shift from “before” to “after” is not just healing—it’s rediscovering courage when life feels most fragile.
Awareness and timing decide survival.
Resilience and perspective define recovery.
The real transformation is both physical and emotional.
Next Steps
Know the signs
Sudden groin pain, redness, swelling, or skin changes.
Get emergency help
Go to the ER immediately. Every hour matters.
Follow treatment
Surgeries, antibiotics, and wound care may be needed. Keep all follow-ups.
Support recovery
Counseling, survivor groups, and mental health care are key.
Prevent recurrence
Manage diabetes, weight, and immune conditions. Schedule checkups.
Key point: Fast action creates survival. Ongoing care shapes recovery.
Know the signs
Sudden groin pain, redness, swelling, or skin changes.
Get emergency help
Go to the ER immediately. Every hour matters.
Follow treatment
Surgeries, antibiotics, and wound care may be needed. Keep all follow-ups.
Support recovery
Counseling, survivor groups, and mental health care are key.
Prevent recurrence
Manage diabetes, weight, and immune conditions. Schedule checkups.